Fungal Acne vs. Acne: How to Tell the Difference and Treat It Right
Sometimes persistent pimples aren't what you think...here's how to tell.
Published:
3 minute read
Spoiler alert: fungal acne isn’t really acne. It’s the nickname for a condition called folliculitis — when the hair follicles become infected and form acne-like bumps.
As dermatologist Sandra Lee, MD (aka Dr. Pimple Popper) explains, fungal acne is easy to mistake for the real thing — which is why so many people end up frustrated when their acne treatments don’t seem to work. In this article, we’ll break down how to tell the difference, what causes it, and how to finally clear it up.
Fast facts: fungal acne
- Caused by yeast (Malassezia), not bacteria
- Breakouts are small, uniform bumps that often itch
- Common after sweating, humid weather, or antibiotics
- Needs antifungal care — not typical acne products
Article Quick Links
What causes fungal acne?
Normally, your skin keeps Malassezia yeast in check. But under certain conditions, it can multiply and trigger folliculitis:
- Excessive moisture: humid weather, sweaty clothes, tight-fitting fabrics
- Medications: antibiotics can disrupt your skin’s balance
- Diet: sugar and refined carbs can encourage yeast growth
- Immune deficiency: those with lowered immunity are more susceptible
What does fungal acne look like?
Because the bumps resemble whiteheads, folliculitis is often mistaken for acne vulgaris. Key differences:
- Size: bumps are usually uniform, unlike acne which varies
- Itching: fungal acne often itches; bacterial acne usually doesn’t
- Clusters: fungal breakouts appear in groups, not as isolated pimples
- Color: bumps are redder and more inflamed than typical whiteheads
“The most telling sign isn’t what you see, it’s what you feel,” says Dr. Lee. “Fungal acne itches — that’s your skin signaling this isn’t the same inflammation we see with typical acne.”
Skin conditions that look like fungal acne
Other issues can mimic folliculitis. Here are some common ones:
- Acne vulgaris: presents with pimples, blackheads, and whiteheads. Often improves with benzoyl peroxide. Try: SLMD Acne System, Body Acne System.
- Ingrown hairs: red, inflamed bumps caused by trapped hairs. Prevented with exfoliation. Try: SLMD Body Smoothing System, BP Acne Spot Treatment.
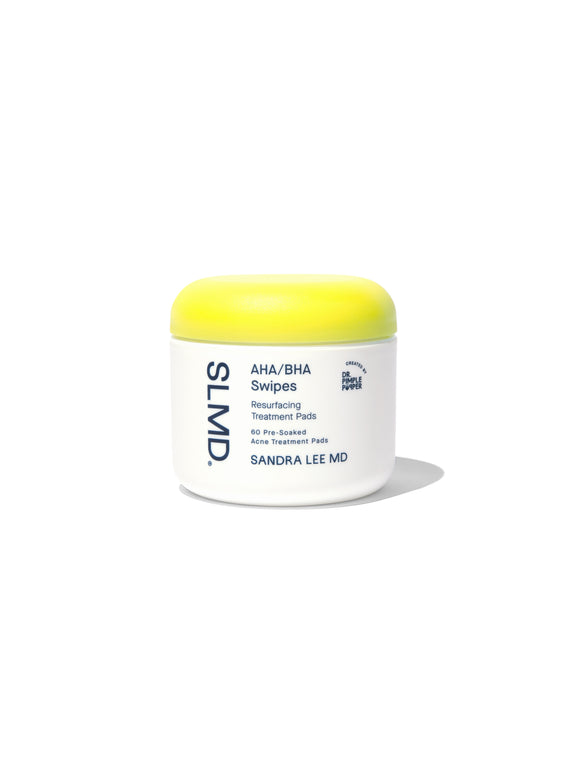
- Milia: tiny white cysts under the skin, often near the eyes. Usually harmless, but exfoliants can help. Try: SLMD SA Acne Spot Treatment, AHA/BHA Swipes, Retinol Resurfacing Serum.
- Contact dermatitis: itchy, red bumps from allergens or irritants. Requires soothing, anti-inflammatory care.
Dr. Pimple Popper's Body Acne & Ingrown Hair Solutions
How do you treat fungal acne?
Traditional acne treatments — like benzoyl peroxide or antibiotics — won’t clear fungal acne, and can sometimes make it worse. If you suspect fungal folliculitis, talk to your dermatologist.
Options that work include:
- Lifestyle changes: shower after sweating, wear breathable fabrics
- Dandruff shampoo: body washes with zinc pyrithione or selenium sulfide
- Antifungal creams: OTC options like clotrimazole or miconazole
- Prescription antifungals: oral medications like fluconazole for persistent cases
How to prevent folliculitis
Fungal acne can come back if the conditions that allow yeast to thrive don’t change. That’s why prevention is just as important as treatment. Small adjustments to your daily routine can make a big difference:
- Use dandruff shampoo as a weekly body wash
- Shower daily and after workouts
- Choose cotton or moisture-wicking fabrics
- Limit excess sugar and refined carbs
- Keep your skincare barrier balanced with gentle hydration
Frequently asked questions about fungal acne
Q: Is fungal acne contagious?
A: Fungal acne, also called folliculitis, is not contagious. It’s caused by an overgrowth of yeast that naturally lives on your skin — not something you can “catch” from someone else.
Q: How do you know if acne is fungal or bacterial?
A: Unlike bacterial acne, fungal acne usually appears as small, uniform bumps that often itch and form in clusters. If your breakouts don’t improve with traditional acne treatments like benzoyl peroxide, that’s a sign it may be fungal. A dermatologist can confirm with an exam or test.
Q: Can fungal acne be treated naturally?
A: Lifestyle changes can help manage fungal acne, including showering after workouts, wearing breathable fabrics, and reducing excess sugar in your diet. But most cases also need antifungal ingredients — either in medicated shampoos, creams, or prescriptions from a dermatologist.
Q: How long does fungal acne take to clear?
A: With the right antifungal treatments, fungal acne often improves within a few weeks. More stubborn cases may take longer or require prescription oral medication, but most patients see relief once the condition is properly diagnosed.

Dr. Lee's Last Word
Fungal acne is frustrating because it looks so much like acne, but it doesn’t behave the same way. With the right diagnosis and antifungal treatment, most patients see improvement quickly.