What Is Acne Vulgaris? A Dermatologist’s Guide to Causes and Treatment
Everything you need to know about the most common skin condition in the world.Published:
5 minute read
Acne vulgaris: it’s the complicated-sounding name for what most of us simply call acne. The term acne comes from the Greek word akné (possibly a typo for akmé), while vulgaris is Latin for “common” or “ordinary.” Put it together, and acne vulgaris refers to the most typical type of acne — the one almost everyone deals with at some point.
According to Sandra Lee, MD (aka Dr. Pimple Popper), understanding acne vulgaris is key to managing breakouts effectively. Not sure what type of acne you’re dealing with? Here's how to tell if you’re facing blackheads, whiteheads, or more severe pimples. For now, let’s dive into the science behind acne vulgaris and why it happens, so you can better manage your skin.
Article Quick Links
What is acne vulgaris?
Acne vulgaris is an inflammatory disorder of the pilosebaceous unit, also known as the pore. Each pore contains three main components:
- Hair follicle: Specialized cells that produce hair proteins.
- Arrector pili muscle: Responsible for making hair stand on end (goosebumps).
- Sebaceous gland: Produces sebum, a natural oil that’s excreted into the pore.
Acne vulgaris occurs when the delicate balance of this system gets disrupted. This can result in two main types of acne:
- Non-inflammatory acne: Clogged pores caused by a buildup of dead skin and sebum.
- Inflammatory acne: When bacteria in the pore trigger inflammation.
Key point: Acne vulgaris arises from disruptions in the pore’s function, leading to both clogged pores and inflammation.
What are the symptoms of acne vulgaris?
The symptoms of acne vulgaris range from mild to severe and depend on the type of breakout. These can occur on any area of the body with active sebaceous glands, such as the face, chest, and back.
Non-inflammatory lesions
- Blackheads: Open clogged pores with a dark surface caused by oxidation.
- Whiteheads: Closed clogged pores trapped beneath the skin’s surface.
Inflammatory lesions
- Papules: Small, red bumps that feel tender or sore.
- Pustules: Pimples filled with pus, surrounded by redness.
- Nodules and cysts: Large, deeper, and often painful lesions that can scar if untreated.
Key point: Symptoms of acne vulgaris range from mild clogged pores to severe inflammatory lesions, requiring tailored treatment based on the type and severity.
What causes acne vulgaris?
While the exact mechanisms behind acne aren’t fully understood, dermatologists believe it stems from a combination of factors:
Sebum: More than just excess oil
People with acne-prone skin tend to produce more sebum, but that’s only part of the story. Research shows that the composition of sebum in acne patients differs from that of acne-free individuals. Certain compounds in sebum, like triglycerides and squalene, may damage the skin barrier, create oxidative stress, and provoke inflammation.
Keratin: The clog culprit
Keratinocytes (skin cells that produce keratin) play a key role in acne formation. In acne-prone skin, these cells undergo hyperkeratinization, causing too much keratin to build up in the pore. This leads to clogs by:
- Producing excess skin cells
- Holding onto dead skin cells longer than normal
Bacteria: The inflammatory trigger
The bacterium Cutibacterium acnes (formerly Propionibacterium acnes) is a natural resident of everyone’s skin. However, in acne-prone individuals, this microbe can overgrow in clogged pores, disrupting the skin’s microbiome and triggering an immune response that leads to inflammation.
Key point: Acne vulgaris results from a combination of excess sebum, hyperkeratinization, and bacterial overgrowth that disrupts the skin’s natural balance.
How do you treat acne vulgaris?
Acne vulgaris affects people of all ages and can vary from mild to severe. The best treatment depends on the type of acne you’re dealing with. Combining targeted treatments is often the most effective approach.
Non-inflammatory acne (blackheads and whiteheads)
Managing non-inflammatory acne focuses on clearing clogged pores and preventing future buildup. Dr. Lee recommends:
- Salicylic acid: This beta hydroxy acid penetrates deep into the pores to dissolve oil and dead skin, effectively reducing blackheads and whiteheads. Try: SLMD Salicylic Acid Cleanser, Salicylic Acid Spot Treatment, Salicylic Acid Pimple Patches, Salicylic Acid Body Spray
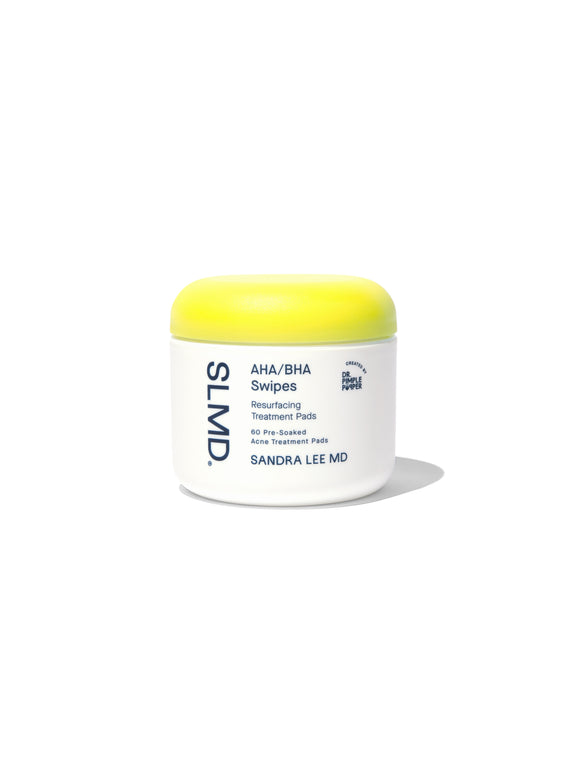
- Glycolic acid: An alpha hydroxy acid that exfoliates the skin’s surface, breaking down dead cells to improve texture and prevent clogged pores. Try: SLMD AHA/BHA Swipes, Glycolic Acid Body Scrub
- Retinoids: These vitamin A derivatives increase cell turnover, keeping pores clear while also improving skin texture and minimizing early signs of aging. Try: SLMD Retinol Resurfacing Serum
Inflammatory acne (papules, pustules, cysts, and nodules)
For inflamed and red breakouts, treatments focus on calming irritation and reducing bacteria. Dr. Lee recommends adding these additional ingredients:
- Benzoyl peroxide: An effective antibacterial ingredient that targets C. acnes, reduces inflammation, and helps clear existing breakouts while preventing new ones. Try: SLMD Benzoyl Peroxide Acne Lotion, BP Body Wash, BP Acne Spot Treatment
- Sulfur: A natural mineral that absorbs excess oil, inhibits bacterial growth, and soothes irritated skin, making it ideal for sensitive, inflamed areas.
- Retinoids: These powerful ingredients regulate skin cell turnover and reduce inflammation, helping to treat deeper pimples while minimizing the risk of future breakouts and scarring.
Key point: Tailor your acne treatment to the type of breakouts you have—exfoliants for clogged pores, antibacterial agents for inflammation, and retinoids for long-term management and prevention. A complete routine (like SLMD Acne System) can target every stage.
Dr. Pimple Popper answers acne vulgaris FAQs
Q: What’s the difference between acne vulgaris and cystic acne?
A: Acne vulgaris is an umbrella term for common acne, which can include blackheads, whiteheads, and inflamed pimples. Cystic acne is a severe form of acne vulgaris that involves deep, painful cysts caused by intense inflammation.
Q: Does everyone get acne vulgaris?
A: Most people experience acne vulgaris at some point, especially during puberty. However, some individuals are genetically less prone to acne due to differences in skin type, oil production, or immune response.
Q: Is acne vulgaris the same as hormonal acne?
A: Hormonal acne is a subset of acne vulgaris caused by fluctuations in hormones, such as during puberty, menstrual cycles, or menopause.
Q: Can diet affect acne vulgaris?
A: While diet isn’t a direct cause of acne vulgaris, high-glycemic foods and dairy may exacerbate acne in some individuals.

Dr. Lee's Last Word
Acne vulgaris is the most common type of acne, affecting people of all ages. Whether you’re dealing with blackheads, whiteheads, or inflamed red pimples, there are effective dermatological ingredients to help manage breakouts. The key is starting with a consistent skincare routine tailored to your needs. Avoid popping your pimples, and remember to be patient and gentle with your skin — it takes time to see results.