5 Types of Acne Scars & How To Treat Each One
Dr. Pimple Popper explains why acne scars form and what can actually help.
Published:
7 minute read
Acne scars come in different forms, and not all of them respond to the same treatments. Here, dermatologist and SLMD Skincare founder Sandra Lee, MD (aka Dr. Pimple Popper) breaks down the five main types of acne scars and how they’re typically treated, as well as steps that can help prevent new ones from forming.
Fast Facts: Acne Scars
- Acne scars form when inflammation disrupts normal skin healing
- Atrophic scars look indented; hypertrophic ones are raised
- Hyperpigmentation after acne is discoloration, not a true scar
- Early, consistent acne treatment helps prevent permanent scarring
- Some in-office procedures can improve the look of scars
#1 Ice pick scars
Ice pick scars form when your skin loses collagen and the overlying skin collapses, leaving a deep depression that looks like a tiny hole. These scars tend to be narrow but extend deeper into the skin, which is why they can be challenging to treat.
- Scar type: atrophic (aka depressed/sunken)
- What it looks like: deep, pinpoint pits that almost look like someone took a tiny needle and punctured your skin
- Who’s affected: people prone to severe, deep cystic acne, typically on the jawline, chin and cheeks due to hormonal changes
How do you treat ice pick acne scars?
Because ice pick scars extend deeper into the skin, they’re typically treated with in-office procedures performed by a dermatologist. Common options include:
- Chemical peels: high-strength peels induce a controlled “burn” that prompts skin to remodel and can soften the edges of scars over time (must be performed by a trained professional)
- Punch grafting: the scar is removed with a tiny circular tool and the opening is filled with a skin graft, usually taken from behind the ear
- Punch excision: the scar is cut out and the edges are sutured together, leaving a flatter, finer line
Preventing new ice pick scars starts with getting severe acne under control early. Dermatologists often recommend a consistent, multi-step acne routine to minimize inflammation and deep breakouts.
Try: SLMD Acne System, Body Acne System
Dr. Pimple Popper's Acne Treatment Picks
#2 Boxcar scars
When you have inflammatory acne — red, inflamed, irritated papules, pustules, or cysts — boxcar scars are an unfortunately common aftermath. They tend to be shallow to medium-depth, but they have sharper edges than rolling scars.
- Scar type: atrophic
- What it looks like: round or oval depressions with sharp, vertical edges, reminiscent of chicken pox scars
- Who’s affected: people with inflammatory, cystic acne, especially on the cheeks and temples
How do you treat boxcar acne scars?
Boxcar scars can often be improved with a combination of resurfacing and volume-restoring procedures. Depending on depth and location, dermatologists may use:
- Punch excisions — the indented portion of the scar is removed and the edges are sutured together to close the gap
- Dermabrasion — mechanical resurfacing of the skin with an ablative instrument under local or general anesthesia
- Fillers — temporary (like Juvederm or Restylane), semipermanent (such as Bellafill), or autologous fat transfer can be injected to raise indented scars to the level of the surrounding skin
Consistent acne control — and avoiding pimple picking — can lower the risk of new boxcar scars forming in the first place.

#3 Rolling scars
If your skin has undulating scars with soft, smooth “shoulders” — the dermatologist’s term for edges — you may have rolling acne scars. These scars tend to become more noticeable with age, as skin loses its natural tightness and elasticity.
- Scar type: atrophic
- What it looks like: shallow, wave-like, saucer-shaped scars
- Who’s affected: generally, people with long-term inflammatory acne; more common in men
How do you treat rolling acne scars?
Rolling scars often respond well to treatments that stimulate collagen and break up tethered scar tissue. Options can include:
- Microneedling — devices with multiple tiny needles create micro-injuries that stimulate collagen production and smooth the skin’s surface over time
- Subcision — a sharp needle is inserted under the skin to release fibrous bands that are pulling scars downward
- Lasers — resurfacing lasers remove or heat the top layers of the skin to encourage collagen remodeling (usually requires multiple sessions and some downtime)
At home, keeping acne under control with a dermatologist-approved routine is key to preventing additional rolling scars from developing.

#4 Keloid scars
Keloid scars are mounds that form when the body’s healing response goes into overdrive after inflammation or injury. Instead of stopping once the wound is repaired, your skin continues to produce collagen and scar tissue, creating a raised, sometimes itchy or tender scar.
- Scar type: hypertrophic (aka enlarged/raised)
- What it looks like: discolored, bumpy or puffy raised scars that may extend beyond the original breakout area
- Who’s affected: all skin types, but more common in darker skin tones; may run in families
How to treat keloids
Keloid scars can be frustrating to treat, because they have a tendency to come back. Dermatologists typically use a stepwise approach, such as:
- Cortisone shots — corticosteroid injections help break down collagen and reduce scar tissue, though not all keloids respond equally
- Lasers — certain lasers can help improve the color and texture of keloids that have already been softened with injections
- Retinoids — topical vitamin A derivatives (like OTC retinol or prescription tretinoin) may be used on thickened areas once the keloid has been reduced
- Surgery — hypertrophic scars like keloids can be surgically removed, but because they frequently recur, many dermatologists prioritize non-surgical options first
If you’re prone to keloids, talk to your dermatologist before getting piercings, tattoos, or elective procedures, since any skin trauma can trigger new scars.
#5 Hyperpigmentation (not a true acne scar)
Hyperpigmentation is often mistaken for acne scarring, but it isn’t a true scar. Instead, it’s discoloration that develops after a pimple heals, appearing as flat pink, red, tan, or brown marks on the skin. These marks form as part of the body’s inflammatory response and are commonly referred to as post-inflammatory hyperpigmentation (PIH) or, when redness lingers, post-inflammatory erythema.
Unlike true acne scars, hyperpigmentation does not involve permanent damage to the skin’s structure. The skin remains smooth, and these marks typically fade over time.
- Scar type: not a true scar (discoloration only)
- What it looks like: flat red, pink, brown, or purple marks left behind after a pimple heals
- Who’s affected: all skin types, though more common in people with darker skin (more melanin) or those who tan easily
How do you treat hyperpigmentation after acne?
Because hyperpigmentation sits on the surface rather than altering skin texture, treatment focuses on supporting even skin tone and preventing marks from getting darker or lingering longer than necessary.
- Daily sunscreen to prevent worsening discoloration. Try: SLMD Daily Moisturizer with SPF 15
- Consistent acne control to reduce new inflammation. Try: SLMD Benzoyl Peroxide Acne Lotion + Retinol Resurfacing Serum
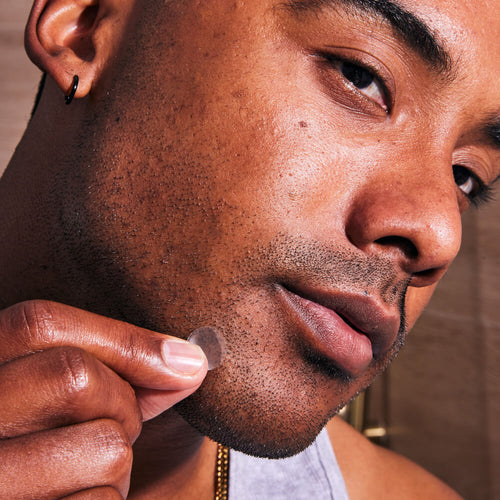
- Gentle exfoliation and retinoids to support skin turnover. Try: SLMD AHA/BHA Swipes
- Avoiding picking or irritating healing blemishes
With patience and sun protection, most hyperpigmentation gradually fades — sometimes completely — making this the most manageable and least permanent of post-acne skin changes.
A note about acne scarring from Dr. Pimple Popper
"One of the hardest parts of acne scarring isn’t what you see in the mirror, it's how it can make you feel. I want patients to know that struggling with confidence because of acne is incredibly common, and it’s something we can talk about just as openly as treatment options."
Frequently asked questions about acne scars
Q: Can acne scars go away on their own?
A: True acne scars that change the texture of your skin — like ice pick, boxcar, rolling, or keloid scars — typically do not disappear completely on their own. However, discoloration after acne often fades over time, especially when you protect your skin from the sun and use brightening ingredients as directed.
Q: What is the best way to prevent acne scars?
A: The most important step is to treat acne early and consistently, using dermatologist-approved ingredients like salicylic acid, benzoyl peroxide, and retinoids. It’s also crucial not to pick, squeeze, or pop pimples, since trauma makes scarring more likely.
Q: Are at-home treatments enough for acne scars?
A: Skincare alone can help support healthy-looking skin and fade discoloration, but it has limits when it comes to true scar tissue. Many people with moderate to severe acne scarring need in-office procedures, like lasers, microneedling, fillers, or surgical techniques, to see more dramatic improvement.
Q: Should I treat acne scars while I still have active breakouts?
A: Dermatologists usually focus on clearing active acne first, then target scars once breakouts are under better control. That said, you can still use daily sunscreen and gentle brightening ingredients to help minimize dark marks as you go, as long as they fit with your acne routine.
Q: When should I see a dermatologist about my acne scars?
A: If scarring or discoloration is bothering you (especially if it’s affecting your confidence) it’s a good time to check in with a board-certified dermatologist. They can identify your scar type, recommend realistic treatment options, and help you build a routine that also prevents future scarring.

Dr. Lee's Last Word
Acne scarring is something I talk about with patients every day. The good news is that there are real options, and even small changes can make a big difference in how people feel about their skin.